A new study reveals a novel gene associated with major depression. The research, published in the April 28 issue of the journal Neuron, suggests a previously unrecognized mechanism for major depression and may guide future therapeutic strategies for this debilitating mood disorder.
|
|
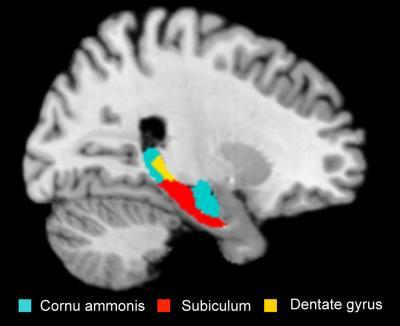
| Depressive patients carrying the risk allele show volume reduction in certain regions of the hippocampus. (Credit: MPI for Psychiatry) |
Major depression is a psychiatric disorder that is responsible for a substantial loss in work productivity and can even lead to suicide in some individuals. "Current treatments for major depression are indispensible but their clinical efficacy is still unsatisfactory, as reflected by high rates of treatment resistance and side effects," explains study author Dr. Martin A. Kohli from the Max Planck Institute of Psychiatry in Munich, Germany. "Identification of mechanisms causing depression is pertinent for discovery of better antidepressants."
While is likely that a combination of genetic and environmental risk factors contribute to major depression, identification of risk-conferring genes has been challenging due to the complexity of the genetics and the considerable environmental factors associated with the disease. Dr. Kohli and colleagues performed a stringent genome-wide association study of patients diagnosed with major depression and matched control subjects with no history of psychiatric illness. They identified SLC6A15, a gene that codes for a neuronal amino acid transporter protein, as a novel susceptibility gene for major depression. The finding was confirmed in an expanded study examining over 15,000 individuals.
The researchers examined the functional relevance of the genetic association between SLC6A15 and major depression. Already nondepressed subjects carrying the risk-conferring genetic variants showed lower expression of SLC6A15 in the hippocampus, a brain region implicated in major depression. Moreover, using human brain imaging, risk variant carriers with a positive life history of major depression showed smaller hippocampi. Finally, in a mouse model, lower hippocampal SLC6A15 expression was linked to the effects of chronic social stress, a proven risk factor for depression.
The authors suggest that reduced SLC6A15 expression might lead to perturbation of neuronal circuits related to susceptibility for major depression. "Our results support the notion that lower SLC6A15 expression, especially in the hippocampus, could increase an individual's stress susceptibility by altering neuronal integrity and excitatory neurotransmission in this key brain region," says senior author Dr. Elisabeth B. Binder. "Because SLC6A15 appears amenable to drug targeting, our results may incite the discovery of a novel class of antidepressant drugs."